Benefit plans are sometimes confusing and employees might be struggling to understand what an employer offers them. This Know Your Benefits flyer lists common terms used in the health insurance industry and explains each in detail. Click for a PDF to download and share with your employees today!
Stimulus Bill Extends FFCRA Tax Credits but Not Leave Mandate
An appropriations bill, which was signed into law on Dec. 27, 2020, does not extend the employee leave mandates created by the Families First Coronavirus Response Act, which expire on Dec. 31, 2020. However, the bill extends tax credits for employers who offer the leave through March 31, 2021.
While employers are no longer required to offer the extensive medical leave benefits for COVID-related absences defined under the original FFCRA, the stimulus will provide credits for employers if they decide to extend this offer to them through March 31, 2021. You can read the full bulletin here: Stimulus Bill Extends FFCRA Tax Credits but Not Leave Mandate
Affordable Care Act Compliance Notes – Jan. 6, 2021
The ACA requires employers to report the cost of group health plan coverage on employees’ Forms W-2. This ACA Overview explains the W-2 reporting requirement, including its application to small and large employers. Affordable Care Act Compliance Notes – 6 Jan 2021
How a Biden Administration Might Impact HR and the Workplace
While we don’t have a Magic 8 ball, with a new Executive Administration, all signs point to changes to how you approach your human resources. Our seasoned prognosticators have some insight for you.
Each presidential transition brings changes to the HR landscape. And the more prepared an HR team is, the easier it will be for them to succeed amid these changes. To that end, this article discusses potential changes employers can expect during a Biden presidency.
To read more, click the image at right to view the article (PDF) in a new window.
Health Benefits – Information Update – 4/6/2020
By Sherree L. Craig, CEBS


Sherree L. Craig, CEBS
Bravo to the businesses continuing uninterrupted, but changed, right now.
As you may be struggling to maintain your footing in business, your employees need some assurances and an understanding of what might happen with their oh-so-important-now health benefits in the event of a reduction in their work hours, a temporary layoff, a furlough, or if a termination of employment becomes necessary.
• Maine Insurance Code Update. By order of Governor Mills, an employer may continue to insure employees during an interruption to their employment. If an employer chooses this option, this offer must be made to “all affected employees on a non-discriminatory basis.”
• COBRA/mini-COBRA. Federal law requires companies with 20 or more employees to offer continuous group health plan coverage to qualified beneficiaries for a certain period of time, depending on the qualifying event. In Maine, employees working for a company with fewer than 20 employees also have a continuation of coverage opportunity in the event of a temporary layoff. This mini-COBRA protection can extend for up to 12 months and can be paid by the employee or company. The insurance company should be notified of this status change, but the employee’s coverage will be maintained on your group bill. It is important to note that if your company is officially out of business, these options are no longer available.
• Healthcare.gov Special Enrollment Opportunity. Employees should be encouraged to review this chance to enroll on the Federal Healthcare Exchange in a timely manner. The loss of group health insurance is considered a qualifying event (unless for non-payment of premiums). This is the time to enroll and apply for subsidies. It must be done at the termination of the group health coverage or at the end of a COBRA election period. They cannot elect COBRA for a few months and then try to switch to the Exchange.
• MaineCare. Due to the expansion of MaineCare eligibility, many of your employees may find themselves eligible for this program. They may apply for coverage or check eligibility at www.maine.gov/mymaineconnection.
If you have questions about this topic, or other federal requirements for continuation of coverage during a medical leave, I encourage you to reach out to your insurance benefits professional.
Wishing you all the best for your health and success.
Anna Moorman Recognized for 2019 Sales


Anna Moorman
Anna Moorman of Allen Insurance and Financial has been recognized for Medicare supplement sales in 2019 by Anthem, one of the largest Medicare supplement carriers in the state of Maine.
Moorman is one of two agents at Allen Insurance and Financial who specialize in the complex market of Medicare insurance, working with a number of insurance carriers to give customers a range of choices to suit their needs. Moorman has been with Allen Insurance and Financial since 2012.
The Anthem award was announced in Portland on Feb. 25. This is the fifth consecutive year that Moorman has received an award from Anthem for Medicare sales; for 2019 she was named one of Anthem’s top 10 sales leaders.
“This award indicates that Anna’s clients appreciate the way she simplifies the process,” said Michael Pierce, company president. “And that’s key, because our goal is to provide dedicated, one-on-one attention to our Medicare customers, assessing each person’s needs and finding options that will align with their budget and healthcare goals.”
Sherree L. Craig Now Licensed as an Insurance Consultant in Maine


Sherree L. Craig, CEBS
Sherree L. Craig, CEBS, Senior Account Executive in the Benefits Division at Allen Insurance and Financial, is now a licensed insurance consultant in Maine.
“Sherree’s efforts demonstrate her deep commitment to continuing professional development,” said Mike Pierce, company president. “This commitment is important to all of our insurance divisions but it is especially so in the always-changing field of employee benefits.”
Craig holds Fellowship standing in the International Society of Certified Employee Benefit Specialists through the Wharton School of Business, and an advanced certification in self-funding from the National Association of Health Underwriters.
2020 Medicare Parts A & B Premiums and Deductibles
On November 8, 2019, the Centers for Medicare & Medicaid Services (CMS) released the 2020 premiums, deductibles, and coinsurance amounts for the Medicare Part A and Part B programs.
Medicare Part B Premiums/Deductibles
Medicare Part B covers physician services, outpatient hospital services, certain home health services, durable medical equipment, and certain other medical and health services not covered by Medicare Part A.
Each year the Medicare premiums, deductibles, and copayment rates are adjusted according to the Social Security Act. For 2020, the Medicare Part B monthly premiums and the annual deductible are higher than the 2019 amounts. The standard monthly premium for Medicare Part B enrollees will be $144.60 for 2020, an increase of $9.10 from $135.50 in 2019. The annual deductible for all Medicare Part B beneficiaries is $198 in 2020, an increase of $13 from the annual deductible of $185 in 2019.
The increase in the Part B premiums and deductible is largely due to rising spending on physician-administered drugs. These higher costs have a ripple effect and result in higher Part B premiums and deductible.
From day one, President Trump has made it a top priority to lower drug prices. Currently, for Part B, the law requires CMS to pay the average sales price for a drug and also pays physicians a percentage of a drug’s sale price. This incentivizes drug companies to set prices higher and for physicians to prescribe more expensive drugs – because that leads to a higher Medicare payment. Through the President’s drug pricing blueprint, the Trump Administration is working to lower drug prices in Medicare Part B drugs.
CMS is committed to empowering beneficiaries with the information they need to make informed decisions about their Medicare coverage options, including providing new tools to help them make those decisions through the eMedicare initiative. In addition to the recently released premiums and cost sharing information for 2020 Medicare Advantage and Part D plans, we are releasing the premiums and cost sharing information for Fee-for-Service Medicare, so beneficiaries understand their options for receiving Medicare benefits. As previously announced, as a result of CMS actions to drive competition, on average for 2020, Medicare Advantage premiums are expected to decline by 23 percent from 2018, and will be the lowest in the last thirteen years while plan choices, benefits and enrollment continue to increase. Premiums and deductibles for Medicare Advantage and Medicare Part D Prescription Drug plans are already finalized and are unaffected by this announcement.
Medicare Part B Income-Related Monthly Adjustment Amounts
Since 2007, a beneficiary’s Part B monthly premium is based on his or her income. These income-related monthly adjustment amounts (IRMAA) affect roughly 7 percent of people with Medicare Part B. The 2020 Part B total premiums for high income beneficiaries are shown in the following table:
| Beneficiaries who file
individual tax returns with income: |
Beneficiaries who file
joint tax returns with income: |
Income-related monthly adjustment amount | Total monthly premium amount |
| Less than or equal to $87,000 | Less than or equal to $174,000 | $0.00 | $144.60 |
| Greater than $87,000 and less than or equal to $109,000 | Greater than $174,000 and less than or equal to $218,000 | 57.80 | 202.40 |
| Greater than $109,000 and less than or equal to $136,000 | Greater than $218,000 and less than or equal to $272,000 | 144.60 | 289.20 |
| Greater than $136,000 and less than or equal to $163,000 | Greater than $272,000 and less than or equal to $326,000 | 231.40 | 376.00 |
| Greater than $163,000 and less than $500,000 | Greater than $326,000 and less than $750,000 | 318.10 | 462.70 |
| Greater than or equal to $500,000 | Greater than or equal to $750,000 | 347.00 | 491.60 |
Premiums for high-income beneficiaries who are married and lived with their spouse at any time during the taxable year, but file a separate return, are as follows:
| Beneficiaries who are married and lived with their spouses at any time during the year, but who file separate tax returns from their spouses: | Income-related monthly adjustment amount | Total monthly premium amount |
| Less than or equal to $87,000 | $0.00 | $144.60 |
| Greater than $87,000 and less than $413,000 | 318.10 | 462.70 |
| Greater than or equal to $413,000 | 347.00 | 491.60 |
Medicare Part A Premiums/Deductibles
Medicare Part A covers inpatient hospital, skilled nursing facility, and some home health care services. About 99 percent of Medicare beneficiaries do not have a Part A premium since they have at least 40 quarters of Medicare-covered employment.
The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,408 in 2020, an increase of $44 from $1,364 in 2019. The Part A inpatient hospital deductible covers beneficiaries’ share of costs for the first 60 days of Medicare-covered inpatient hospital care in a benefit period. In 2020, beneficiaries must pay a coinsurance amount of $352 per day for the 61st through 90th day of a hospitalization ($341 in 2019) in a benefit period and $704 per day for lifetime reserve days ($682 in 2019). For beneficiaries in skilled nursing facilities, the daily coinsurance for days 21 through 100 of extended care services in a benefit period will be $176.00 in 2020 ($170.50 in 2019).
| Part A Deductible and Coinsurance Amounts for Calendar Years 2019 and 2020 by Type of Cost Sharing | ||
| 2019 | 2020 | |
| Inpatient hospital deductible | $1,364 | $1,408 |
| Daily coinsurance for 61st-90th Day | $341 | $352 |
| Daily coinsurance for lifetime reserve days | $682 | $704 |
| Skilled Nursing Facility coinsurance | $170.50 | $176 |
Enrollees age 65 and over who have fewer than 40 quarters of coverage and certain persons with disabilities pay a monthly premium in order to voluntarily enroll in Medicare Part A. Individuals who had at least 30 quarters of coverage or were married to someone with at least 30 quarters of coverage may buy into Part A at a reduced monthly premium rate, which will be $252 in 2020, a $12 increase from 2019. Certain uninsured aged individuals who have less than 30 quarters of coverage and certain individuals with disabilities who have exhausted other entitlement will pay the full premium, which will be $458 a month in 2020, a $21 increase from 2019.
For more information on the 2020 Medicare Parts A and B premiums and deductibles (CMS-8071-N, CMS-8072-N, CMS-8073-N), please visit:
Rates for Individual Health Insurance Plans via ACA May Drop for 2020
Maine’s three providers of individual health insurance on the Affordable Care Act marketplace have revised their rate requests for 2020, significantly lowering their projected rates.
This is good news for anyone who plans to enroll or to renew their coverage in health insurance via the Affordable Care Act for 2020.
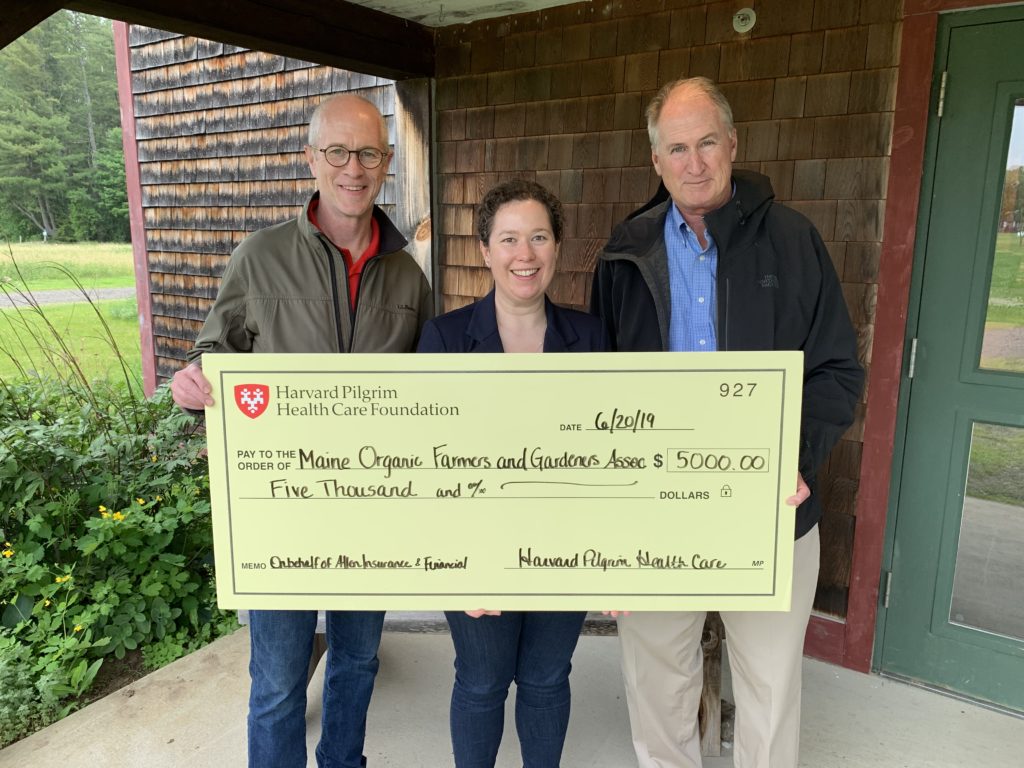
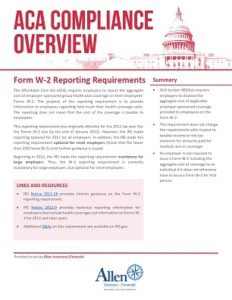
MOFGA Receives Grant from Harvard Pilgrim Health Care and Allen Insurance and Financial
The Maine Organic Farmers and Gardeners Association (MOFGA) recently received a $5,000 grant from Harvard Pilgrim Health Care Foundation and Allen Insurance and Financial to increase access to and affordability of healthy, nutritious food for low income families. MOGFA has a longstanding commitment to help all Maine people acquire local, organic foods regardless of geography or income. Pictured in the photo, left to right, are: Bill Whitmore, Maine Market Vice President, Harvard Pilgrim Health Care; Sarah Alexander, Executive Director, Maine Organic Farmers and Gardeners Association; and Dan Wyman, JD, Insured Benefits Manager, Allen Insurance and Financial.